Pyelonephritis, a common urinary tract infection, can cause severe complications if left untreated. Understanding the symptoms, causes, and risk factors of this condition is crucial for early detection and effective treatment. In this article, we will explore pyelonephritis in detail, including the various diagnostic tests and procedures used for accurate diagnosis. Additionally, we will delve into the strategies and prevention techniques that can help manage and treat pyelonephritis effectively. By the end of this article, you will have a comprehensive understanding of pyelonephritis and be equipped with the knowledge to identify and address this condition promptly.
1. “Understanding Pyelonephritis: Symptoms, Causes, and Risk Factors”
Pyelonephritis is a severe infection of the kidneys that requires prompt diagnosis and treatment. Understanding the symptoms, causes, and risk factors associated with this condition is crucial for early intervention and to prevent complications.
Symptoms:
Pyelonephritis often presents with a range of symptoms that can vary in severity. Common signs include a high fever, persistent back or abdominal pain, frequent urination, and a strong urge to urinate. Additionally, individuals may experience cloudy or bloody urine, fatigue, nausea, and vomiting. In severe cases, patients may develop confusion or delirium, indicating that the infection has spread to the bloodstream. It is important to note that the symptoms of pyelonephritis can resemble those of a urinary tract infection, so a thorough medical evaluation is necessary for an accurate diagnosis.
Causes:
The primary cause of pyelonephritis is a bacterial infection, most commonly stemming from Escherichia coli (E. coli) bacteria. These bacteria typically reside in the gastrointestinal tract but can enter the urinary tract through the urethra and ascend to the kidneys. Factors that increase the risk of developing pyelonephritis include urinary tract abnormalities, such as kidney stones or structural defects, weakened immune system, urinary catheterization, and conditions like diabetes that impair the body’s natural defense mechanisms against infection.
Risk Factors:
Certain individuals are more susceptible to pyelonephritis due to various risk factors. Women have a higher risk than men due to their shorter urethra, which allows bacteria easier access to the urinary tract. Sexual intercourse can also introduce bacteria into the urinary system, increasing the likelihood of infection. Pregnant women face an increased risk as hormonal changes during pregnancy can impair urinary flow and hinder the body’s immune response. Additionally, individuals with a history of recurrent urinary tract infections are more prone to developing pyelonephritis.
It is essential to be aware of these symptoms, causes, and risk factors associated with pyelonephritis. Seeking immediate medical attention if any symptoms arise can prevent the infection from spreading and causing severe complications, such as kidney damage or sepsis. Through early diagnosis and appropriate treatment, individuals diagnosed with pyelonephritis can recover fully and prevent recurrent infections.
You can find out more about this theme here: https://bbgate.com/media/4-mmc-mephedrone-synthesis-complete-video-tutorial.37/.
2. “Diagnosing Pyelonephritis: Tests and Procedures for Accurate Diagnosis”
Diagnosing Pyelonephritis: Tests and Procedures for Accurate Diagnosis
When it comes to diagnosing pyelonephritis, healthcare professionals employ a variety of tests and procedures to accurately identify this potentially serious kidney infection. Since the symptoms of pyelonephritis can overlap with other urinary tract infections, it is crucial to conduct a thorough evaluation to ensure an accurate diagnosis. Here are some commonly used tests and procedures for diagnosing pyelonephritis:
1. Medical History and Physical Examination:
The initial step in diagnosing pyelonephritis involves obtaining a detailed medical history and conducting a physical examination. The healthcare provider will inquire about any symptoms experienced, previous urinary tract infections, kidney stones, or any underlying medical conditions that may increase the risk of pyelonephritis. During the physical examination, the healthcare provider may gently press on the back or abdomen to check for tenderness or any signs of kidney enlargement.
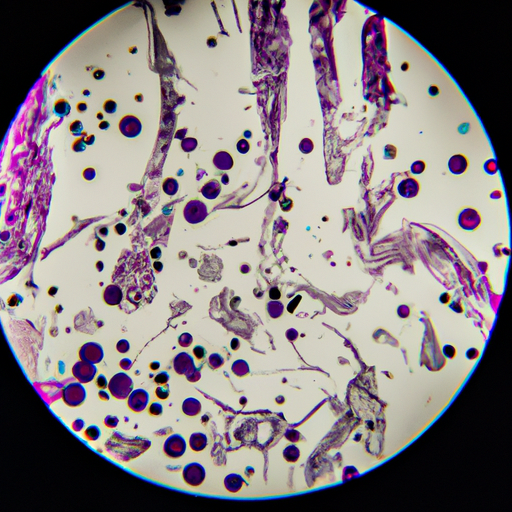
2. Urinalysis:
Urinalysis is a fundamental diagnostic tool used to detect the presence of infection or inflammation in the urinary tract. A urine sample is collected and analyzed to identify the presence of bacteria, white blood cells, red blood cells, and other substances that may indicate an infection. Additionally, the urine may be tested to determine the type of bacteria responsible for the infection, which helps guide appropriate antibiotic treatment.
3. Urine Culture:
A urine culture is often performed alongside urinalysis to determine the specific bacteria causing the infection. This test involves incubating a urine sample to allow the bacteria to multiply, enabling identification and testing for antibiotic susceptibility. The results of a urine culture help healthcare providers select the most effective antibiotic for treatment.
4. Blood Tests:
Blood tests are valuable in assessing the severity of the infection and evaluating kidney function. A complete blood count (CBC) may reveal an increased number of white blood cells, indicating the presence of an infection. Additionally, blood tests can measure kidney function by assessing levels of blood urea nitrogen (BUN) and creatinine. Elevated levels may indicate kidney damage due to pyelonephritis.
5. Imaging Studies:
In certain cases, imaging studies may be necessary to evaluate the kidneys and surrounding structures. These tests help identify any abnormalities or complications associated with pyelonephritis. Common imaging techniques include:
– Ultrasound: This non-invasive procedure uses sound waves to produce images of the kidneys. It can help detect any signs of kidney enlargement, blockages, or abscesses.
– CT Scan: Computed tomography (CT) scans provide detailed cross-sectional images of the kidneys and urinary tract. They can identify any structural abnormalities,
3. “Treating Pyelonephritis: Effective Strategies and Prevention Techniques”
Pyelonephritis, a severe kidney infection, requires immediate medical attention and appropriate treatment to prevent complications and ensure a full recovery. The primary goal of treating pyelonephritis is to eliminate the infection, relieve symptoms, and prevent the infection from spreading to other parts of the body. Here, we will explore effective strategies and prevention techniques for managing pyelonephritis.
1. Antibiotic Therapy:
The cornerstone of pyelonephritis treatment is antibiotics. Prompt administration of appropriate antibiotics is crucial to combat the underlying bacterial infection. The choice of antibiotics depends on the severity of the infection, local resistance patterns, and individual patient factors. Typically, oral antibiotics are prescribed for mild to moderate cases, while severe cases may require intravenous antibiotics in a hospital setting. It is essential to complete the full course of antibiotics as prescribed by the healthcare provider, even if symptoms improve before completion.
2. Adequate Hydration:
Maintaining proper hydration is vital during pyelonephritis treatment. Drinking plenty of fluids helps flush out bacteria from the urinary tract and kidneys, reducing the risk of reinfection. Water is the best choice, but other fluids like herbal teas and non-caffeinated beverages can also contribute to hydration. It is advisable to avoid alcohol and caffeinated drinks as they can irritate the bladder.
3. Pain Management:
Pyelonephritis often causes severe pain and discomfort. Over-the-counter pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help alleviate pain and reduce fever. However, it is essential to consult a healthcare professional before taking any medication, as some individuals may require alternative pain management strategies due to underlying medical conditions or contraindications.
4. Hospitalization and Intravenous Fluids:
In severe cases of pyelonephritis, hospitalization may be necessary. Hospitalization allows for closer monitoring of the patient’s condition and facilitates intravenous administration of fluids and antibiotics. Intravenous fluids help ensure adequate hydration and promote faster recovery. Hospitalization is particularly crucial for individuals with additional risk factors, such as pregnancy, compromised immune systems, or underlying kidney diseases.
Prevention Techniques:
1. Practice Good Hygiene:
Maintaining good personal hygiene is essential to prevent urinary tract infections (UTIs) that could potentially lead to pyelonephritis. This includes regularly washing the genital area, especially before and after sexual intercourse, and wiping from front to back after using the toilet to prevent the spread of bacteria from the anus to the urethra.
2. Urinate Regularly and Completely:
Avoid holding urine for prolonged periods as this can